The recent attention to the crisis in long term care, and nursing homes by the White House is long overdue, dearly wanted and potentially disastrous; careful what you wish for! Nursing homes and long-term care have been largely ignored or been given passing attention for decades.

The “Fact Sheet” issued by the Biden Administration is a good example of public opinion polling, punitive attention and lack of awareness among the political class of the real facts. Resident / family advocacy groups will find the demands for increased staffing as causes for celebration; they too should be careful what they wish for. Operators will have a very different response, since the additional requirements will be costly, and there is little expectation of additional funding. Much of what was announced by the White House and by the President in his State of the Union Speech is punitive.
Owner/operators of skilled nursing centers, especially family-owned and not-for-profit nursing homes, will suffer the most if the regulations envisioned by the “Fact Sheet” are promulgated, implemented and enforced.
The devil in the details
There are #21 recommendations that break down into #3 categories
- Staffing requirements
- Performance
- Transparency
Here are the actions anticipated by the White House “Fact Sheet”
| 1. Minimum Staffing Standards | 2. Reduced crowding – more private rooms |
| 3. Reduce costs; value-based payment | 4. Further decreases in antipsychotic use |
| 5. Increase inspections | 6. Ratchet down on poor performers |
| 7. Increase penalties | 8. Ownership transparency |
| 9. “Technical Assistance” | 10. National database of ownership |
| 11. Ownership | 12. Bolster Nursing Home Compare |
| 13. Research private equity | 14. Affordable Aide Training |
| 15. Improve workforce sustainability. | 16. National Career Pathways |
| 17. Continued COVID-19 testing in long-term care facilities. | 18. Continued COVID-19 vaccinations |
| 19. Strengthen Requirements – Infection Preventionists. | 20. Enhance Requirements for Preparedness. |
| 21. Integrate Pandemic Lessons |
Given the starting point with regard to nursing homes, none of this seems unreasonable. However, the devil is in the details here.
Staffing
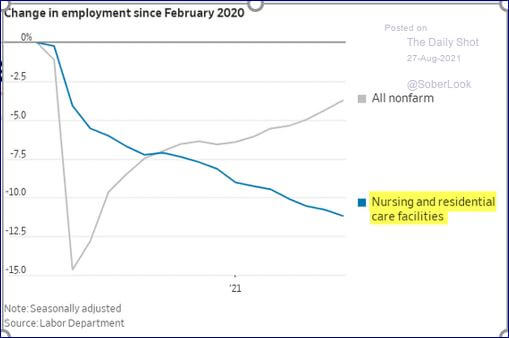
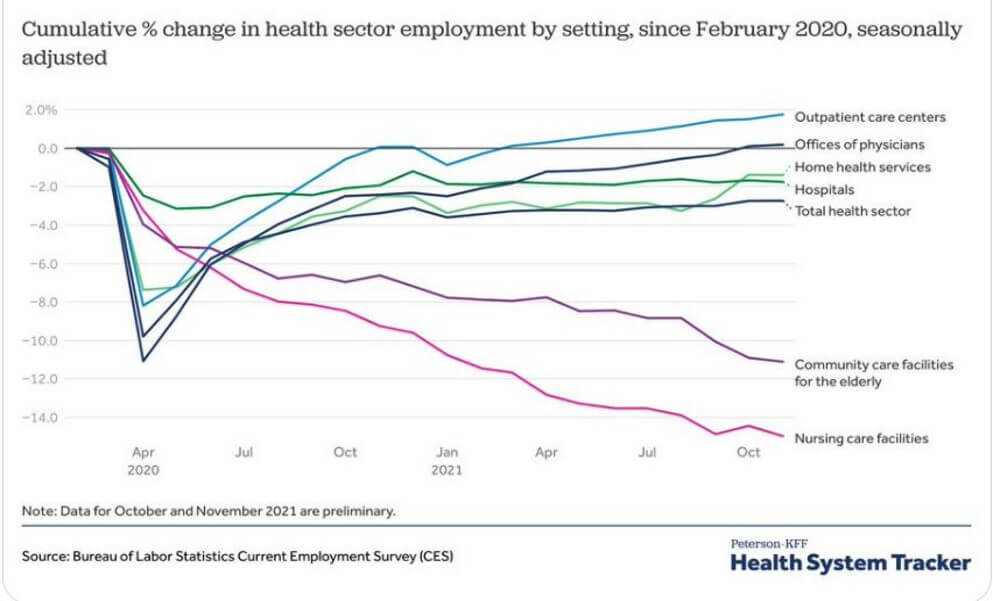
Long-term care is in the midst of its worst staffing crisis ever.
In the United States, there are ~500,000 fewer frontline workers employed in long-term care than there were at the start of the pandemic. It has been assumed that more caregivers equals better care and increased staffing has been used as a proxy for quality improvement.
The empirical evidence about this is mixed, and what is more likely is that other variables than raw numbers or ratios are more correlated with quality.
States which have implemented minimum staffing requirements, especially since the start of the pandemic, have had to back off, or use waivers because of the desperate shortage of frontline workers.
No one is happy about this staffing crisis.
Currently, nursing homes are rated on a star rating system, and the most important standard is staffing. Most nursing homes, in most locations around the United States are unable to staff at levels which would allow them to be rated as five-star (the highest rating). This is not because they cannot pay enough (although they can’t) it is, rather, because the staff simply aren’t there. In part because of the pandemic, qualified staff have gone to work other places – outpatient clinics, hospitals and doctors’ offices.
For the White House to suggest that nursing homes will be required to hire staff that don’t exist, and then penalized when they fail guarantees even more bankruptcies than have already occurred.
If it were possible to hire more staff, many nursing homes would.
 One suggestion is that owners don’t hire more people to keep costs down and thereby increase profit. This might have been the case in some buildings before the pandemic but there are owners and executives pushing trays in kitchens and changing linens in patient rooms because there simply isn’t anyone else to do it!
One suggestion is that owners don’t hire more people to keep costs down and thereby increase profit. This might have been the case in some buildings before the pandemic but there are owners and executives pushing trays in kitchens and changing linens in patient rooms because there simply isn’t anyone else to do it!
If a standard is impossible to achieve (like hiring more staff), then what purpose does it serve?
There are also hopeful and sensible suggestions which would benefit the residents of nursing homes and improve the supply of staff over the intermediate and longer-terms. For example, the White House Fact Sheet calls for affordable nurse’s aide training, career pathways for the direct care workforce, and steps toward workforce sustainability. All of these are advisable, in addition to immigration reform and a renewal of the foreign nurses’ Visa program.
Performance
The performance of nursing homes in their fundamental task – caring for and protecting vulnerable persons – is difficult to measure. As I and others have written about, both the qualitative and quantitative measures of nursing home performance are difficult. Either they are peremptory or missing entirely. Most of what is referred to as performance improvement standards for nursing homes in the existing body of law and regulations are really efforts to control for, monitor and correct deviations. Of the eight (8) suggestions about performance in the White House Fact Sheet, one has to do with physical crowding (calling for private rooms), one has to do with reducing costs (calling for an expansion of Value-based Payment) and the third calls for further reductions in the use of antipsychotic medications, while five (5) are additional “controls” which are clearly designed to be punitive. In balance, this formula of sector regulation is sure to have the opposite effect of what is needed and intended.
Transparency
Removing the opacity associated with nursing home ownership and investment is long overdue. Too often, nursing home assets are passed into the hands of disinterested, and occasionally nefarious actors. This is exactly the proper role for the federal government; to cut through the bureaucratic nexus of state and federal regulations to expose ownership and, therefore, responsibility. It is unfortunate that the sector has become identified with these actors.
An Alternative Fact Sheet
The real facts of the current state of nursing homes are these:
- Nursing homes have been systematically ignored and underfunded for 40 years; there should be no surprise that they are in a dreadful state;
- Nursing homes lose money on over half of their residents; 66% of nursing home residents are paid at 68% the cost of caring for those residents;
- Since the start of the pandemic, nursing homes and residential care homes have lost almost 500,000 frontline workers;
- In most marketplace areas, unemployment is so low, and competition for entry-level workers so high, that nursing homes are unable to compete for low-wage, frontline workers;
- Multiple occupancy rooms are standard in nursing homes, encoded in the Medicaid payment regulations, not an “option”; calling for private rooms is gratuitous because countless operators would be bankrupt within a few weeks if they complied;
- Private equity, pilloried by the president in the SOTU speech, is invested in approximately 5% of the total inventory of 15,269 nursing centers; the harms cited are based on a microscopic sample, and the research cited is not conclusive.
Investment
 The deepest concern is that there is no proposal by the White House to create new investments in the sector. This is naked ageism.
The deepest concern is that there is no proposal by the White House to create new investments in the sector. This is naked ageism.
The penetration of private equity in the sector is growing, and if there are concerns, now is the time to make rational policy-based regulations about such investments. However, as is mentioned above, the inventory of nursing homes in the United States is decrepit. There are two ways to fix this – debt or equity. Since most nursing homes operate with only a few weeks cash on hand, it is highly unlikely that taking on debt is a possible or approvable approach to upgrading the infrastructure. Equity investments seem the logical path, if you conclude that nursing homes are enterprises and therefore subject to the same financing requirements of other businesses. How will these investors achieve their return on investment?
Among the investments which need to be encouraged by federal and state governments is far more, empirically based research in nursing homes. For example, “more staff equals better quality” has not been empirically proved in repeatable, robust research. Maybe it’s not the number of staff deployed, but which staff, at what time and where, that are more important? And there’s currently no national database of qualitative information that would allow research or benchmarking for quality of life, or family and resident satisfaction.
These investments are not included in the White House’s calls for action. It appears that long-term care, and especially nursing homes will continue to reflect society’s widespread ageism. What is needed in addition to what the White House has proposed is a path forward with structured investment in nursing home and long-term care infrastructure, as well as staff.
——————————————————————————————————————————
Irving Stackpole is President of Stackpole & Associates, a marketing, market research and training firm at www.StackpoleAssociates.com. He can be reached directly at: istackpole@stackpoleassociates.com.
Ramona Backhaus, Hilde Verbeek, Erik van Rossum, Elizabeth Capezuti, Jan P.H. Hamers, Nurse Staffing Impact on Quality of Care in Nursing Homes: A Systematic Review of Longitudinal Studies, Journal of the American Medical Directors Association, Volume 15, Issue 6, 2014, Pages 383-393, ISSN 1525-8610, https://doi.org/10.1016/j.jamda.2013.12.080.
(https://www.sciencedirect.com/science/article/pii/S1525861013007962)
Backhaus, R., Beerens, H.C., van Rossum, E. et al. Rethinking the Staff-Quality Relationship in Nursing Homes. J Nutr Health Aging 22, 634–638 (2018). https://doi.org/10.1007/s12603-018-1027-3
Karen Spilsbury, Catherine Hewitt, Lisa Stirk, Clive Bowman, The relationship between nurse staffing and quality of care in nursing homes: A systematic review, International Journal of Nursing Studies, Volume 48, Issue 6 2011, Pages 732-750, ISSN 0020-7489, https://doi.org/10.1016/j.ijnurstu.2011.02.014.
(https://www.sciencedirect.com/science/article/pii/S0020748911000538)

