Date: 8th September 2021
To watch the recording click here
Register to download the webinar presentation.
Transcript
Epilogue to a Crisis
Facilitated by Irving Stackpole.
This presentation is designed to focus on issues that relate to the Long-Term Care story that’s playing out in the post-Cold War era, in the post-Pandemic time period. I’m going to focus on how we got here, what the situation is, and leave some time at the end for what I hope will be your questions. So let me launch in here and talk about long term care. So the plot for this storyline this week, I’ve talked about an epilogue, but the plot for the basic storyline is that nursing homes or Congregate Care homes or residential care facilities (depending on where you’re located) – they came out of poor houses. They were designed to be replacements to poor houses. Over time, the plot line goes, those nursing homes, congregate care centers, care homes. They got old and we stopped building new ones, especially in the United States as well as in the UK and other locations. Then nobody wanted to work there. And I’ll talk more in detail about that and the government regulators, said Highmore. So we paid the people that work in these congregate care centers poorly and then we told them to do even more. So you can see that this plotline is full of contradictions, paradoxes and conflicting intentions. And then we had Covid, which was an enormous jolt to the system.
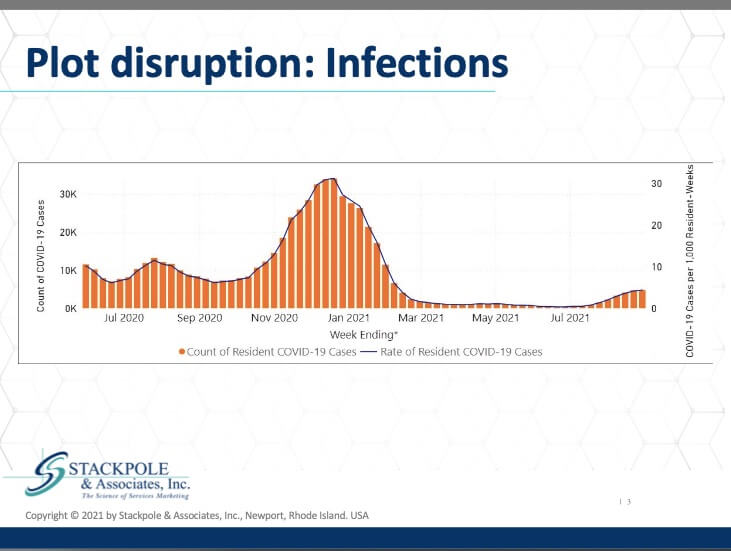
Here are the infections that occurred in the US in nursing homes. This data is from CMS. As we can see, the infections were very, very serious from November through the beginning of March 2021. And now, infections have gone up a little bit further with the Delta variant spreading throughout the communities in which these nursing centers are located. Deaths; equally disturbing numbers, a very significant rate of death associated with Covid-19 in nursing homes. The situation in nursing homes has gotten significantly better. But again, Delta has spread in the communities where the nursing homes are located. The staff and employees in these nursing centers live in the communities, and they almost invariably have an effect on the spread of the disease in nursing centers. So now we run into the epilogue.
Well, what’s an epilogue? It’s some sort of “afterwards”, or some sort of finale or supplement to the storyline. I think in order to properly draft it, we have to consider that it is indeed a crisis and that the epilogue is to this crisis. So a crisis is an adverse event – certainly we’d all all agree that the pandemic is that – and it had a tremendous impact on the brand and the sector in its entirety. So the storyline continues; the epilogue in congregate long term care certainly will continue. There are market segments that I would say are durable. That is to say, there are individuals and situations where the services of congregate long term care centres will be necessary in skilled nursing and nursing homes. But basically it’s those who have no choice. And these people who have no choice are individuals who are generally poor, generally very sick, and they have neurological disorders that require intensive nursing and personal care support and/or they have memory loss or cognitive impairment (which is not dementia). These individuals will continue to require congregate care and no amount of rhetorical pleading or wishful thinking, among other things, will change that fact. It’s an epidemiological fact in Western populations. These are diseases of the age that are associated with aging; they come with aging and we have an aging society. So we’re going to experience a higher incidence and overall burden of these types of diseases as we progress, especially over the next 8 to 12 years. So these are the folks who will continue to need or require nursing homes, as well as assisted living and home care.
In other programs, I’ve talked about the market share between and among these various segments, and if you have questions about that, I’d welcome the opportunity to respond to them as a strategist. I want to focus on congregate care right now and we’ll talk a little bit about other forms of congregate care later, but specifically the most intense: generally referred to as nursing homes, nursing care, care homes and skilled nursing.
So the characters in this story, in this long term care story, and there’s a set of characters, we can weave a plot with them. The first is the markets. The markets are the people who currently need or may require congregate long term care in the future. There’s the physical structure to which these individuals are referred, or the physical structures where they seek residential care. There’s the programmed structure, what we do collaboratively on their behalf inside of these structures. Then there’s technology and information, what little of it there is inside of these structures, and then there’s workforce – we’ll be drilling down into this significantly. In econometric terms, the workforce in long term care is the “means of production”. It’s how we produce the care that’s delivered in these congregate care centers. There’s the culture, which are the unspoken norms that bind our behaviors together. Within these structures, there are the outcomes – what are the results of what we do? And we’ll talk about that as well. And then there’s economics. Most people flee to one or two or three of these subjects based on their interests, based on the topic at hand. But all of these are critical characters in the long term care story. And if we’re going to approach the epilogue to this crisis, we need to take all of these characters into account. We need to make sure that each of them comes onto the stage afterward for a bow when the play is successful.
So where are we in the congregate housing and long term care markets? As you can see, as you track with these numbers, this data is pretty consistent, the Covid pandemic has dropped the demand right off the cliff. It seems to be coming back in certain areas. Some of the comeback story is wishful thinking, but in general, the pandemic has seriously negatively impacted the demand, the occupancy utilization, if you will, of congregating long term care housing in the United States. Some of it will come back and we have done a prior webinar on what segments will come back first and how they’ll come back. I would refer you to that if that’s of interest to you. But this is only one of the characters in this story – the markets and where we are now. This was to be predicted. This is not a surprise. The various forces in the plot had been conspiring for some time to reduce the demand, specifically in nursing homes in both the US and the UK, reduced demand for nursing homes through regulation, through preferred programs and regulatory structures, payment options that would encourage the utilization of home and community based services versus “institutional care” in congregate care. 
And those effects pre-Covid were pretty effective, as you can see here for the past 35 years, utilization in the 65+ age category, which is a pretty big lump and not a way I would recommend looking at markets in general, but this is the available data that we had there. CMS has gone from 5.2% to 2.35%. That’s a pretty significant drop in the utilization of a category of service among that particular market segment. And the reasons for that are manyfold, but the overall demographic of demand in aged care services is driven by the number of age qualified individuals.
And as we can see here from this table, this is the United States live births from 1900 to 2010, and as we can see, from 1925 to roughly 1940, there was a significant dip in the live births in the United States. This demographic dip has had a significant impact on the demographic demand for aged qualified housing and services. And I’ve inserted some lines and boxes here to show that in 2022, if you were born in 1935, you will be 87 years of age and as you can see, we’re still in the trough of that demographic dip. It begins to emerge roughly around 2030 – 2035, when we will see an increase in demand based on demographics. The type of demand will be quite different and we’ll touch upon that when we talk about the next steps in this epilogue.
The next character in our play is structure, the physical structures. And this article that appeared in The New Yorker magazine, The American Nursing Home is a Design Failure is cited in the bibliography that’s attached to the program that you will receive for signing up. The structure of the American nursing home is terrible. The property, plant and equipment, which was the original PPE – most nursing homes were built between 1960 and 1965. What do I mean by most? Over 70%. They were modeled on hospitals and they were built with the same cookie cutter modern era nod to efficiency, attempting to create, hub and spoke distribution of the patients in these buildings. They were different from assisted living. Assisted living is much newer, and didn’t reach the United States until the early 1990s. But there hasn’t been new construction in nursing homes in the United States since roughly 1985 – 1987. And that’s in part due to conditions; sort of certificate of need restrictions that are almost ubiquitous throughout the United States. So there’s barriers to building new nursing homes, which has been a boon in many ways to assisted living since the mid-70s, early 80s, there’s been little or no reinvestment in nursing centers. It’s true that there have been upgrades and paint jobs and new awnings, but there’s been very little reinvestment for major capital improvements. And the reason for that is most of the capitalization in the sector has been extractive – it’s been built around the real estate that undergirds the properties, and the federal government has withdrawn the kind of fiscal support needed to make low cost loans available for major physical revisions, major physical reengineering like new HVAC systems, new physical entrances, new windows which all bare upon the Covid pandemic. As we know now, the SARS-COV-2 microbe spreads through aerosols, aerosols that were aided and abetted by the limited ancient HVAC systems in these buildings. And the result? Yuck. I have probably been in 3,000 nursing homes around the United States and another hundred or so in the UK as well as elsewhere in the world, and I can tell you that I wouldn’t want to stay in a Hilton that hadn’t been renovated for 40 or 50 years, would you? They are too often very grim.
So what do we need? First of all, we need a much wider variety of physical structures. Right now, the payment systems, especially in the United States, conspire to restrict the type of centre where an individual can live and receive care. So those restrictions need to be carefully combed through, eliminated and/or modified without restricting safety. And that can be done. We need large, newer college dormitory-type buildings with attractive common spaces. We need medium-sized buildings like the current assisted living residences, which in the United States average about 70 units per operation. And we need small McMansions for a small, unrelated or related group of individuals. Think Golden Girls – we need those kinds of structures as well.
The physical structures are benchmarked, but there’s little or no qualitative or quantitative analysis of the suitability of these structures; are these structures really fit for purpose, as we say in the UK? In too many cases they are not. But we don’t know. There’s been no predictive analysis done of what consumers or their families want (that we can find). We’re keen to find a sponsor for such a research project. But there’s been no predictive analytics done. There’s been little or no qualitative analysis of consumer, customer, or family satisfaction in congregate long term care, especially nursing homes. We’ve got caps and other things in hospitals, but we don’t have that in long term care. The real estate that undergirds the sector can be both a positive or a negative. Real estate can allow equity investment, which is far more easily handled by the sector than the types of “get investment” that’s simply not available to many nursing centers. We need IT infrastructure, and that’s a capital expense. I consider congregate long term care in the United States and in the UK as the land that IT left behind. It’s embarrassing and I’ll talk further about that. Basically, we need access to capital. And what that means is we need a new federal Hill Burton Act. We need ways for private and public developers to get access to low-interest guaranteed debt where they can reinvest in a meaningful way, or redevelop, or rebuild, or build new and meaningful ways. Small model, medium model and big model. Why don’t we get this? Well, because, frankly, we’ve been too competitive. The sector is so hyper competitive, we’re busy eating each other’s lunch. We’ve focused on profit at the expense, I would say, of the future strategically. And the other issue that needs to get brought up is that (sarcastically) it pays to confuse the consumer. Well, one of the things that we need to understand is that consumers don’t understand the taxonomy or the structure of congregate long term care. They don’t understand the difference between a rehab center and an assisted living residence, between an independent living residence and a specialty care centre. They don’t understand these artificial distinctions. They don’t understand them, frankly, because we have not committed ourselves to educating our markets. But labeling is confusing and that has made this situation, this epilogue all the more confusing. And we as a collective, we don’t bargain together. We haven’t, at least until the pandemic hit. We haven’t collectively bargained and lobbied effectively for the issues that are meaningful and substantive to the sector. More on that soon.
Now to the internal programs. This is Stackpole, my 87 year old pretend mother who’s in a nursing home, and the program that she receives in Boston will be profoundly different from the program she will receive in Dallas, which will again be very, very different from the program she might receive in San Diego. Why is that? She needs the same thing, but the programs are highly fragmented. One of the reasons for that is that the coverage varies. The programs, the insurance programs, the intermediary programs that my mother may qualify for in one place might be very different from what she qualifies for in another place. And what I as her adult child or what her daughter in law may learn about might be different in all three locations. It’s crazy. The graphic here is an attempt to depict the complete mystery that consumers face when they turn to long term care and attempt to figure out how to meet the needs of their aging parents or significant others. There’s issues in the communities, home based care, congregate care, nursing care. How did it get this complicated? Well, my theory is that the government and the regulators, all very well-intentioned perhaps, were attempting to control for fraud or attempting to create audit trails. And so they created silos and never rationalized – to use W. Edwards Deming’s term – those systems between and among themselves. So there’s little or no collaboration, cooperation or rationalization across the system. And if the consumer doesn’t know what she wants or needs, why aren’t we teaching her? Why aren’t we investing in communications and education around the needs for our aging population?
So what do we need? We need first of all, screening and triage. We need a way to screen individuals as to what they need at some entry point in their trajectory, in their journey, in their storyline. What do they need? Do they need behavioral health services? Do they need domestic services? Do they just need grocery delivery? Do they need someone to call and prompt them from time to time? We don’t do anything like that. We need to fit the person to the program, not to the payment. We need to look past the payment silos and look carefully at what the individual needs around the country in the post-pandemic era. There are individuals and organizations, and I’m happy to be part of some of these initiatives, that are attempting to create things that are so sensible, such as beds in congregate care centers that aren’t limited to a particular payment class. In other words, beds that can be used by individuals who need the bed rather than only by individuals who meet certain payment stipulations. And we need clear choices, the overall sector of long term care is more complicated than credit default swaps. And if you haven’t seen the movie The Big Short, I recommend it to you. Finding our way through the maze of long term care is more complicated than that.
Technology and information. There was a public outcry at the beginning of a pandemic about individuals who couldn’t get information. They couldn’t get information; there were immediate lockdowns as a result of the pandemic, and families, regulators couldn’t get information. Well, they couldn’t get information because as they say in Texas, “that dog doesn’t hunt”. There had been no investment in information infrastructure. In fact, long term care centers are specifically excluded from major legislation that invests in health care infrastructure. Why that is, I can only speculate and it’s not flattering. We need to solve that. We need to resolve it. And in some ways, it’s better because we can leapfrog – we can leapfrog right into newer technology. But as I say here on the bottom, Kroger’s, the local department stores, the local grocery stores have better technology than almost every congregate care center.
What do we need? First of all, we need to care more about granny than we do about tomatoes, which means we need to invest in the IT infrastructure in congregate care. And part of that investment is in individuals in the sector; operations managers, administrators, executive directors, CEOs. We need to demand interoperability. We need to demand inexpensive, easily-applied tools within our congregate care centers that will actually improve management, improve efficiency and improve oversight. One of my favorite topics is personal emergency response systems. Everybody says, “Oh, we’ve got PERS; we’ve got personal emergency response systems.” All of these are built on legacy hospital-based systems and telephone systems. We need far more sophisticated systems. We need an Internet of long term care. You’ve heard of the Internet of Things (IoT) – we need an Internet of long term care. We need electronic health records. I’m not eschewing things like PPC or other matrices or other nursing home-based electronic health records. The problem is that those systems are headed in the same way as hospital-based systems. Cerner and EPIC – they don’t talk to each other and that has created major problems. News article just today about a study showing how the reason that information was so slow to start from hospitals at the beginning of the pandemic was because of these conflicts. We have an opportunity to start right – to do it right from the get-go. We need interoperability. I’m doing a project under a Cares Act grant right now in Rhode Island trying to find interoperability solutions, and it is a nightmare.
We need to look at things like ambient assisted living. Ambient assisted living simply means that the tools of surveillance are placed wherever mom or grandma lives and we use those tools to keep an eye on them. That’s what ambient assisted living means, and the technologies are readily available. My company has a patent in this area and I’m not the most technologically sophisticated person – if we can do it, it can certainly be done on a broader scale.
People, the means of production from an econometric point of view, are one of the most important characters in this play in this story line for long term care. Who cares? Well, paid and unpaid caregivers who want to work in the long term care sector. As we will see, the number of people working has dropped. And we need to be far more rigorous about locating, identifying, recruiting and retaining. And I’ve got some thoughts in that regard: what are the sources of these individuals today? And what are the sources of these individuals tomorrow? Well, pre-Covid, the best data was from the Kaiser Family Foundation, which suggested that there were about four and a half million long term care workers in the United States. As I said earlier, the NHS has some analogous information in the UK. Pre-Covid, most of the people working in long term care work in congregate centers, skilled nursing nursing homes and assisted living residences, with about 33% working in home health. These were the facts pre-Covid and then the pandemic hit.
This is data from the Labor Department. And as you can see, nursing and residential care facilities employment since February 2020 has plummeted, whereas all nonfarm employment has recovered very effectively. Now I don’t doubt for a minute that everybody here who’s an operations manager, however many are here, that you are experiencing this at a very painful level; that the nursing and residential workforce has not only decreased, but is also becoming very difficult to recruit within. Why? One of the reasons is absolutely compensation. We have through politics and poor, poor lobbying and a variety of other factors, we have consistently and regularly underpaid our direct care workforce in long term care. This graph says a lot about that, and indeed, this is a big issue. We must find ways to pay what these jobs are worth. We’re migrating quickly from a service based economy to a care economy where care provision will become a dominant element of the economy overall in all of the OECD countries. You just need to look at Japan to see this.
Let’s talk specifically about the workforce in long term care and what might be possible. So who wants to work in long term care? First of all, it’s clear from the data and I’m just going to go back here and show that this data has a bottom, that it’s clear that there are people who really do want to work in long term care. It will take a generation at least, and I would say two generations, to remove the stigma associated with congregate long term care. That is a significant undertaking that needs to recruit the participation and the compensation of interested parties in that endeavor, and I have some suggestions about that as well. But we need to work hard to remove this stigma.
The other thing that we need to do is to be far more rigorous about looking at why people take jobs versus why they stay in jobs versus why they leave jobs. There was very elegant research done in 2016 and some that continues to be done at Brandeis and other other locations such as UMass Boston, about why people leave. But all three of those issues – why people take the job, why people stay in the job and why people leave the job – need to be far more rigorously analyzed so that we can take steps today to concretely improve recruitment and retention, and understand why people leave when they leave so that we can address the issues – if any can be addressed – inside our organizations from a management point of view. We need a federal Long Term Care Jobs Act. We need a program that will stimulate recruiting, compensating and supporting long term care workers throughout the United States. I suggest that since there are a core of at least 10 million un- or underemployed individuals in the United States, we could start there. And we can indeed screen for things like loyalty and compassion and sensitivity, those screenings can produce interest and motivation, as well as begin to chip away at the legacy negative cultural metaphor about long term care. We could use existing federal training centers. There’s no law against this. Federal training centers are deployed throughout the United States. They’re supported under a different title and the federal code, and they can indeed be training centers where technical training or hands-on training can be developed. For those people who screen into the Long Term Care Jobs Act workforce, we just subsidize salaries and benefits at a federal level. The vast majority of individuals who are employed in caregiving roles today are what’s called ALICE: Asset Limited Income-Constrained and Employed. These are people who are within 200% of the federal poverty limit. They’re generally women, and they’re very often working single mothers. There are ways we can support their migration into our workforce and there are ways we can incentivize them to stay in our workforce. These things can only occur with coordinated nationwide effort and we need to reinstate the H1-A visa category for caregivers. This program worked beautifully to bring tens of thousands of nurses into the United States. During the late 80s, the program was disbanded, I think in 1992 or 1993 it ended, but the bottom line is that there is a precedent for creating a category for nursing and other qualified caregivers to bring them into the United States. This is absolutely a high priority because the demographic situation isn’t going to get any better. We’re migrating toward a care-based economy, but there’s not going to be anybody there to care.
Let’s talk briefly about the character of culture in long term care. Right now, the culture is embattled. I would say there is a core of individuals who have endured. We know who they are. We hope and we pray and we act every day to reinforce our respect for these individuals. These are indeed health care heroes, but without some of the other changes that we’ve talked about, the negative culture will return of feeling as though you’re working as a second class professional in a second class sector that isn’t properly funded, isn’t properly reinvested in, isn’t properly respected by government and regulatory authorities. This is draining. It’s wearing on the culture inside congregate long term care centers. And that, ladies and gentlemen, has to change.
One of the final characters in this play is Outcomes, and famously, “what gets measured gets done” – we all know this is true. Clinical results are being exquisitely measured, one would say, by the new standards of reporting. The new MDS categories and the other regulatory standards promulgated by CMS; they’re really quite good. But they only look at part of the picture. The clinical results, which are fundamentally what’s looked at as Long-Term Care Outcomes, is only part of the story. What about quality? Now, let’s be clear: I’m not talking about a subjective perception. When I talk about quality, I’m using W. Edwards, Deming and Juran; a strict definition of quality, the degree to which the service is free of defects that can and should be measured. And currently it’s not. Another aspect to quality has to do with perception, with the subjective observation that’s called consumer satisfaction. What do consumers want? What do they need and what do the families want and need? Now, we’ve already talked about the fact that families and consumers themselves often don’t know what they want or need because we’ve done such a marvelous job of obfuscating, making it less clear what our offerings are that people often don’t know. The bottom line is that we’re not effectively measuring customer satisfaction. Hospitals have something called H-Caps, and a significant proportion of the hospitals across the United States measure the satisfaction of their consumers, their patients, their ambulatory patients, and they measure it using H-Caps or one of the multiple of the dimensions of H-Caps. We don’t have anything like that. Why? Again, I lay this squarely at the feet of lobbyists and individuals who are advocating for the sector. We need to have consistent measures so that we begin to look at the data. We’ve got data that’s isolated in state silos or individual community silos or individual sector silos – that’s not rationalized, itt’s not made readily available for analysts or analysts to do things like predictive modeling. And as I’ve said before, if consumers don’t know what they want, why aren’t we teaching them outcomes? Outcomes would be measurably better if consumers had reasonable expectations, if we were managing those expectations more effectively.
Finally, the economics – and this would take up a whole session on its own, but I’ve purposely left it to the last here. There are indirect and direct costs associated with providing congregate long term care, and I would say categorically: the system has been short-changed for 50 years. We have under invested in both operations and capital investment for years. The Medicaid system in the United States that pays for 68% of congregate long term care can’t afford the system the way it’s currently structured. The Medicare program, which pays for health care for the elderly, backed out of long term care 45 years ago when they saw the demographic trends. They said, “No, we can’t do this”, and they backed down. Now, Medicare will and does pay for short term care, but that represents a sliver of the overall turnover in the congregate long term care sector. Medicare Part C, the so-called Medicare Advantage Programs, are beginning to see more traction in certain types of assisted living, but overall, Medicare does not pay for the services in congregate care centers. The other issue is that too many Americans think that the government will pay for long term care. For years, my firm did the consumer survey for Philips Lifeline. We did about 35,000 or 40,000 surveys among consumers, and invariably, when asked about compensation, people predicted that the government would pay for long term care. And we know that they don’t, or they will, but only in certain prescribed and limited ways. This is a collision course that’s been accelerated in this story about congregate long term care. Private unpaid care is worth about $500 billion dollars in the United States. That is a very amiable, positive and constructive data point. It’s also immensely unfair. It’s immensely vulnerable, and needs to be addressed for overall economic recovery and specifically toward the long term care crisis. Waste, maldistribution, lack of collaboration and fragmentation are the major culprits inside this economic problem, these economic difficulties in this play. Economics is certainly one of the villainous characters in our long term care story.
Here’s some ideas about how to get what we need. First of all, we need federal insurance for long term care. It’s been proposed so many times, it’s always the bridesmaid, never the bride. So we definitely need federal insurance for long term care. Japan did it about 11 years ago. And if Japan, whose demographics are far worse than ours — their demographic cliff is far steeper and their economics are far more inflated than ours have been — if they did it, we can absolutely do it. We need the political will. We need the experts to step forward and explain why this is so important. We need a small increase in the Medicare payroll deduction, and a small means-tested premium progressive on parts A, C and D in Medicare.
Now you’re going to say, “What? Where did that come from?” The funding for the federal insurance for long term care cannot simply be scraped over onto the backs of the prime age workforce in the United States. It won’t cut it. It isn’t cutting it. Yesterday, Boris Johnson proposed a major reform to social care. It’s already getting appropriate blowback. We’ve got to stop nibbling around the edges and start rebuilding from the ground up. Private long term care insurance is partially deductible now. It needs to continue to be fully deductible, although for a variety of reasons, it’s never going to reach a higher penetration rate than, say, 11% or 12%, which was the peak before Covid and before the long term care insurance providers started to fall out of the marketplace. We need to create a long term care risk pool in each state similar to what ACA did. And we need to require that participating health insurance providers who decide to offer federally-backed insurance for long term care spend a small percentage of their premiums on education and communications to teach consumers what they need, how to get it, where they go to get it, and the difference between memory loss and Alzheimer’s and the difference between an unsupervised congregate care, independent living age, qualified property and a nursing home. Currently consumers don’t recognize this difference. And to those who say, “How can we afford all of this?” I’m simply going to quote John Maynard Keynes, an economist for those of you who don’t know, who basically designed the economic system that pulled the world economy out of the mire and the muck of post-World War II. John Maynard Keynes said, “Assuredly, we can afford this and much more”. Anything we can actually do, we can afford. And all of the things that I’ve suggested here, we can actually do. I believe that we actually must do them, and stop nibbling around the edges.
The next steps. Well, they are to hear your questions, field your questions, to continue the dialogue and the conversation with politicians, regulators and leaders in the sector to redesign and reimagine long term care. The world is the product of our thinking; we can’t change the world, we can’t change this system without changing our thinking. I hope this has been interesting and perhaps even provocative. The resources are attached here, and with that, I would love to see what questions you might have.
Question: Can you talk about the recent tragedies in Louisiana?
Irving: I think that the question has to do with the immediate and swift removal of aged and vulnerable consumers from nursing homes in the path of Hurricane Ida and the placement of these individuals in shelters. My observation about this is two-fold. One is, it has to be considered an emergency evacuation under duress, and I’m sure that the people who did that have the best of intentions. Could it have been done better? Absolutely. They’re “coulda, woulda, shoulda”. What I would have done is put an RFID bracelet on every single consumer and I would have scanned that bracelet into a database, and then I would have hustled those vulnerable individuals in their gurneys, in their wheelchairs, into the best, most suitable destinations I could find for them. But that requires pre-planning, and just as we encountered Sandy in Florida, we are encountering the same issue with Ida in Louisiana, and in New Jersey, by the way, as well. This is the result of the lack of planning and the lack of awareness around the needs of these vulnerable populations. This reflects, frankly, the generally low priority that these sectors have. I know that every politician who heard me say that will immediately get their dander up. But we are the poor stepchildren in congregate long term care, there’s just ample evidence and this is further evidence (of that). So I don’t know what else I can say about that other than just say this is a great example of how we need technology, how we need planning, and how, given what we know about the frequency of these intense extreme weather events, we need to be far better prepared.
Question: What was your reaction, and the pros and cons of the announcement that the US World and News Report will be conducting surveys and publishing rankings of IL, AL, memory care and CCRCs?
Irving: Thank you, that’s a good question. I consider such rankings as beauty contests. I consider such rankings as good public relations. Those of you who score well in these programs should indeed leverage them. I encourage my clients to do that all the time from a public relations perception point of view. But they are fundamentally just that. They are beauty contests. They have nothing to do with the underlying issues. I think I read that the system will rely in part on the CMS star rating system for long term care centers. And we know there are flaws, there are issues with the star rating system, which could be the subject of another conversation. But the fact that the U.S. News and World Report saw an opportunity in this says, “Why? Why aren’t we doing it? Why isn’t CMS doing it? Why isn’t ACHCA or AHCA or Leading H? Why isn’t somebody already doing it?” I suspect it’s because there’s low priority, no funding, and the interests of the private parties, the for-profit vendors of these surveys, and I know because we are one and have been one, they have argued against this or lobbied against it. And we really need systematized metrics that we can use. So that’s my reaction to it.
Question: Isn’t a critical component of transformation the marriage of universal health care and the baseline care coordination IT nationwide a first step? (Note Grundy’s recent New Yorker article on Costa Rica).
Irving: Those are two very good points, but I think they’re inverted. I think that the first thing to do is to create an I.T. infrastructure in long term care. That infrastructure can and will have ripple benefits that are and will be significant. Second of all, there’s a gray line between health care and congregate long term care. There’s quite a few medical services that are delivered within a congregate setting, but there are other segments of the population utilizing congregate centers that don’t require intense medical services. They require social, psychological, or behavioral interactions to help improve their well-being rather than specific medical services. I’m very familiar with Costa Rica, I’ve been there at least eight or nine times working with the healthcare system there. But I think that the questioner order of importance is inverted. I think it needs to be IoT first, the internet of things first, and then other things will follow.
Question: Currently long term care facilities are in competition for qualified and licensed staff due to the staff shortages caused by the Covid-19 pandemic. What can long term care facilities do to stay competitive? Staffing agencies are offering ridiculous rates that long term care providers cannot match due to declining census and our major source of reimbursement, MediAid.
Irving: This reminds me immediately of a famous movie called There Will Be Blood, where one oil wildcatter drilled a horizontal pipeline to another oil wildcatters field and basically sucked all the oil out – this is what’s happening in marketplace areas and even across the country. If I were not ethically concerned about my operation, I would do what many providers are currently doing, which is offering whatever it takes, including suggesting that I would take unvaccinated health care professionals and pay them staggering bonuses so that I would benefit from their services, because after all, I can’t deliver any services if I don’t have those individuals. Those individuals are my means of production. Those of you who are old enough to remember should recall that after World War II, because labor was so short, there were actually compensation restrictions, which is in part how health insurance became such a popular benefit (because it was a non-compensatory benefit that could be added in order to attract workers from contiguous areas or related industries). So this is a workforce crisis, and these bonuses that are being offered are nothing short of a race to the bottom – it’s irresponsible. And the best solution to this is to stop it. Absolutely stop it. And at the state level, to create compensation structures, ladders, caps, whatever you want to call it. Yes – I’m talking about meddling in the free labor market, because it’s not free! There’s a limited supply of the means of production, and the absence of these means of production means that somebody dies, or doesn’t get care, or has to be shipped from one state across state lines to go to another place. We wouldn’t tolerate this with ICU beds. Why should we accept it when it comes to market rates for the workforce? That’s my considered point of view, not my opinion. My considered point of view about the workforce is that there needs to be coordinated federal but state-based action to control these predatory, irresponsible behaviors.
Oh, that’s a great note to end on. Thank you very much and thank you all for attending today’s webinar. We hope you found it informative. Thank you again, everyone. And we look forward to seeing you at the next program. Have a great day, evening and stay well everyone.
Resources
- Williams, B. Failure to Thrive? Long-Term Care’s Tenuous Long-Term Future.
See: https://scholarship.shu.edu/shlj/vol43/iss2/3/ - True, S. et al. COVID-19 and Workers at Risk: Examining the Long-Term Care Workforce.
- Stackpole, I. Bridging the Divide: Transitions to Cross-Continuum Collaborations in Healthcare.
See: https://stackpoleassociates.com/transitions-cross-continuum-collaborations-healthcare - Adoption factors associated with electronic health record: www.ncbi.nlm.nih.gov › pmc › articles › PMC4316426
- Who Cares? The pandemic shows the urgency of reforming care for the elderly. The Economist.
- Jan 28, 2015 – Long-term care (LTC) facilities (as defined by the ARRA) are facility types excluded from the incentives including: skilled nursing homes, assisted … also a source of statistical inference when ‘meaningful use’ is assessed. See: Final Report of NH Commission Public Release Case.pdf
- Coronavirus Commission on Safety and Quality in Nursing Homes. September 2020.
Stackpole & Associates is a marketing, research & strategy consulting firm focused on healthcare and seniors’ services markets. Irving can be reached directly at istackpole@stackpoleassociates.com.